Genotype 3 HCV Mental Health Impact Calculator
Mental Health Risk Assessment
Key Symptoms for Genotype 3 Patients:
Depression
Reported in 45% of genotype 3 patients
Anxiety
Affects ~38% of patients
Cognitive Fatigue
Brain fog can persist months post-treatment
Sleep Issues
Often tied to cytokine peaks at night
Quick Summary
- Genotype3 chronic hepatitisC is linked to higher rates of depression, anxiety, and cognitive fatigue than many other HCV genotypes.
- Virus‑induced inflammation, liver‑brain signaling, and side‑effects of older therapies all play a role.
- Modern direct‑acting antivirals (DAAs) dramatically reduce viral load and improve mental‑health scores, but residual symptoms can linger.
- Regular screening, early counseling, and lifestyle tweaks cut the risk of long‑term psychological impairment.
- Seek professional help if mood changes, suicidal thoughts, or severe brain fog persist after cure.
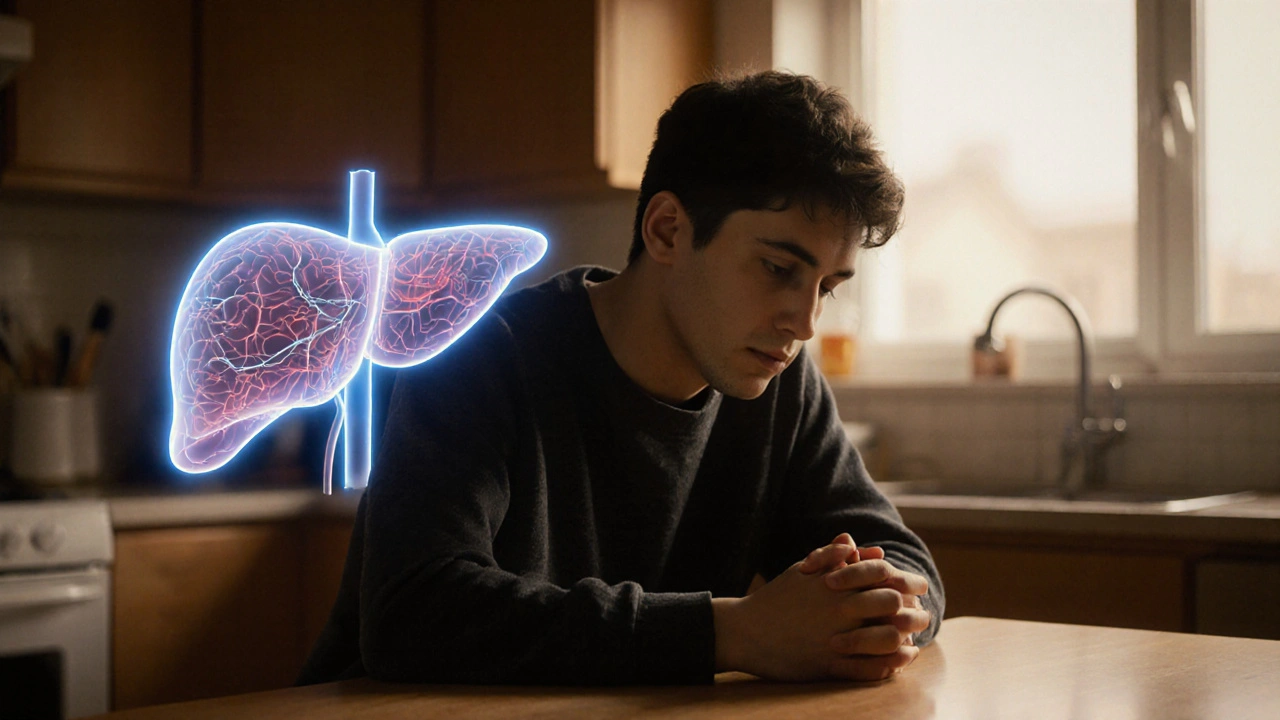
What Is Genotype3 Chronic HepatitisC?
When we talk about Genotype3 chronic hepatitisC is a subtype of the hepatitis C virus (HCV) that primarily affects the liver and is known for faster disease progression and higher rates of liver fat accumulation. It accounts for roughly 30% of global HCV infections, with hotspots in South‑Asia, parts of Europe, and NewZealand’s Pacific communities.
Unlike the more common genotype1, genotype3 carries a higher propensity for metabolic disturbances, which can echo into the brain via inflammatory pathways. Understanding its unique profile is the first step toward grasping why mental‑health outcomes differ.
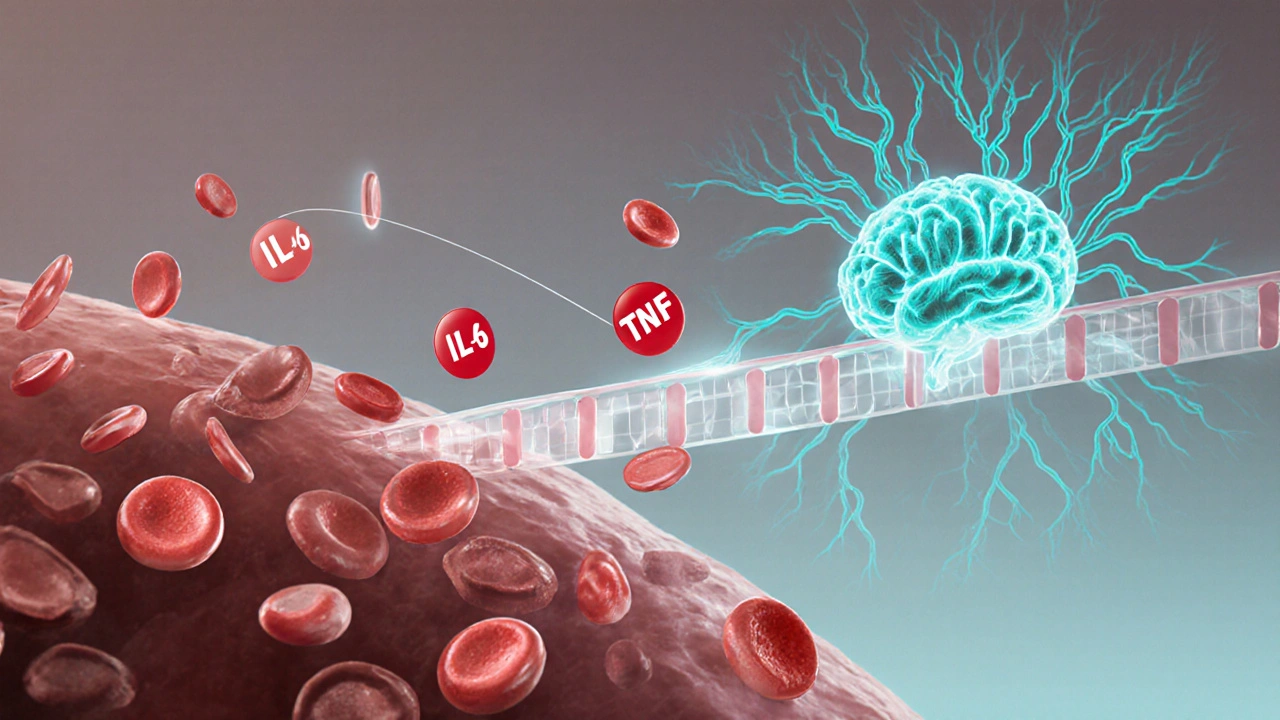
How HCV Reaches the Brain
The hepatitis C virus itself rarely crosses the blood‑brain barrier, but it triggers a cascade of immune signals that do. Elevated cytokines - especially interleukin‑6 (IL‑6) and tumor necrosis factor‑α (TNF‑α) - travel through the bloodstream and activate microglia, the brain’s resident immune cells. This neuroinflammatory response can alter neurotransmitter balance, leading to mood swings, anxiety, and a feeling of “mental fog.”
When liver function declines, toxins such as ammonia build up, further stressing the central nervous system. This liver‑brain axis is especially pronounced in genotype3 because the strain promotes steatosis (fatty liver), worsening metabolic stress.
Typical Mental‑Health Issues Linked to Genotype3
Research from hepatology centers in 2023‑2024 shows a clear symptom pattern:
- Depression - reported by 45% of genotype3 patients, versus 30% for genotype1.
- Anxiety - affecting roughly 38% of those infected.
- Fatigue and cognitive impairment - a “brain fog” that can last months after viral clearance.
- Sleep disturbances - insomnia or fragmented sleep, often tied to cytokine peaks at night.
These issues are not merely reactions to a chronic illness; they stem from measurable biological changes that genotype3 amplifies.
Why Genotype3 May Be Worse for the Mind
Two core factors set genotype3 apart:
- Higher inflammatory load: Studies using ELISA assays found IL‑6 levels 1.8‑times greater in genotype3 patients compared with genotype1.
- Metabolic strain: The virus induces steatosis in up to 70% of carriers, raising insulin resistance and further fueling inflammation.
Both pathways converge on the brain, creating a perfect storm for mood disorders. The table below summarizes prevalence data gathered from three large cohort studies (n≈2,500) across Europe and Oceania.
| Genotype | Study‑Average Prevalence | Sample Size |
|---|---|---|
| 1 | 30% | 1,200 |
| 2 | 28% | 400 |
| 3 | 45% | 800 |
| 4 | 32% | 100 |
Modern Treatment: Direct‑Acting Antivirals (DAAs) and Mental Health
Since the approval of sofosbuvir‑based regimens in 2015, the therapeutic landscape has shifted dramatically. DAAs target viral proteins, achieving cure rates above 95% in genotype3 without the interferon‑related neurotoxicity that plagued older regimens.
Key benefits for mental health:
- Rapid viral suppression reduces cytokine storms within weeks.
- Side‑effect profile is mild - most patients report only headache or fatigue, not mood swings.
- Post‑treatment quality‑of‑life (QoL) scores rise by an average of 12 points on the SF‑36 mental‑health subscale.
However, the cure does not guarantee instant psychological recovery. Residual brain fog can linger for 3‑6months, and pre‑existing depressive disorders may need separate attention.

Practical Steps to Protect Your Mental Well‑Being
- Screen early and often: Use the PHQ‑9 questionnaire at diagnosis, during DAA therapy, and three months after SVR (sustained virologic response).
- Integrate care: Ask your hepatologist to refer you to a mental‑health professional familiar with chronic liver disease.
- Adopt anti‑inflammatory habits: Mediterranean‑style diet, regular aerobic exercise, and adequate sleep lower IL‑6 levels.
- Stay connected: Join peer groups - many online forums (e.g., HCV‑NZ) share coping strategies specific to genotype3.
- Mind‑body techniques: Meditation, yoga, and progressive muscle relaxation have demonstrated modest reductions in HCV‑related anxiety.
When to Seek Immediate Help
If you notice any of the following, reach out to a mental‑health professional or emergency services without delay:
- Sudden increase in depressive thoughts or suicidal ideation.
- Severe, persistent confusion or disorientation.
- Uncontrolled insomnia combined with panic attacks.
- Significant decline in daily functioning despite viral cure.
Early intervention can prevent a short‑term mood swing from becoming a chronic condition.
Frequently Asked Questions
Does curing genotype3 hepatitisC erase all mental‑health problems?
Cure eliminates the viral trigger, so most inflammation‑driven symptoms improve. However, long‑standing depression or anxiety may persist and often benefit from counseling or medication.
Are DAAs safe for people with a history of depression?
Yes. DAAs have a low neurotoxic profile. Doctors usually continue existing antidepressants, and regular mood monitoring is advised during the 8‑12‑week course.
How often should I be screened for depression while on treatment?
A baseline PHQ‑9 at diagnosis, a mid‑treatment check at week4, and a final assessment at the end of therapy are recommended. Follow‑up at three months post‑cure helps catch lingering issues.
Can lifestyle changes alone improve my mood while living with genotype3?
Lifestyle tweaks can lower inflammatory markers and boost energy, but they work best alongside professional mental‑health support, especially if symptoms are moderate to severe.
Is brain fog after HCV cure permanent?
Most patients report gradual improvement over 3‑6months. Persistent cognitive issues beyond six months should be evaluated for other causes, such as medication side‑effects or co‑existing conditions.





Comments
Johanna Sinisalo
October 9, 2025 AT 19:13 PMTake care of your mental health, you’re not alone.
OKORIE JOSEPH
October 10, 2025 AT 14:06 PMThis whole mental‑health hype around genotype 3 is just another excuse for pharma to sell… you think you’re special when you’re just a data point
Lucy Pittendreigh
October 11, 2025 AT 09:00 AMPeople need to stop glorifying their suffering; it’s not a badge of honor. The stats are there, let’s act on them, not just post sad memes.
Nikita Warner
October 12, 2025 AT 03:53 AMWhen evaluating the impact of genotype 3 chronic hepatitis C on mental health, it is essential to consider both the biological mechanisms and the psychosocial context. The virus stimulates cytokine release, particularly interleukin‑6 and tumor necrosis factor‑α, which cross the blood‑brain barrier and activate microglial cells. This neuroinflammatory cascade can disrupt neurotransmitter homeostasis, leading to depressive and anxious symptomatology. Moreover, hepatic insufficiency results in the accumulation of neurotoxic substances such as ammonia, further impairing cognitive function. Studies from 2023‑2024 consistently report a depression prevalence of approximately 45 % among genotype 3 patients, markedly higher than the 30 % observed in genotype 1 cohorts. Anxiety follows a similar pattern, affecting roughly 38 % of this population. Fatigue and the so‑called “brain fog” often persist for several months after sustained virologic response, suggesting that viral clearance does not instantly reverse neuroinflammation. Sleep disturbances, frequently linked to nocturnal cytokine peaks, exacerbate daytime fatigue and mood swings, creating a vicious cycle. Direct‑acting antivirals (DAAs) have dramatically improved virological outcomes, achieving cure rates above 95 %, and they generally possess a benign neuropsychiatric side‑effect profile. However, the residual inflammation and metabolic derangements induced by genotype 3 can linger, underscoring the need for ongoing mental‑health monitoring. Routine screening with tools like the PHQ‑9 at diagnosis, mid‑treatment, and three months post‑cure is recommended to identify patients who may benefit from early psychiatric intervention. Lifestyle modifications-such as adopting a Mediterranean diet, engaging in regular aerobic exercise, and ensuring adequate sleep-have been shown to reduce systemic inflammation and may attenuate depressive symptoms. Finally, integrating hepatology care with mental‑health services, ideally through a multidisciplinary clinic, facilitates timely referrals and personalized treatment plans. By addressing both the virological and psychosocial dimensions, clinicians can mitigate the long‑term mental‑health burden associated with genotype 3 hepatitis C.
Liam Mahoney
October 12, 2025 AT 22:46 PMLook, the data is crystal clear – genotype 3 patients have higher IL‑6 levels and more steatosis – so it’s no surprise they feel worse mentally. If you’re not seeing the link, you’re just ignoring the science, plain and simple.
surender kumar
October 13, 2025 AT 17:40 PMOh sure, because every time I read a medical article I’m just waiting for the next plot twist – “Will the brain fog finally lift after the cure?” Spoiler: it might, but let’s not pretend it’s a magic wand. The drama of chronic illness is real, but playing it up for clicks is tired.
Justin Ornellas
October 14, 2025 AT 12:33 PMGrammar matters: “genotype 3” should be lowercase “genotype 3” when used as a descriptor. Also, the phrase “brain fog” is a colloquialism that, while vivid, lacks the specificity desired in a scientific context. Precision in language mirrors precision in treatment-both are essential.
JOJO Yang
October 15, 2025 AT 07:26 AMSeriously, the emotional roller‑coaster of living with genotype 3 is *the* plot of my life. One day I’m hopeful because DAAs are amazing, the next I’m drowning in fog and feel like the universe is mocking me. It’s like a soap‑opera, except nobody gave me a script.
Faith Leach
October 16, 2025 AT 02:20 AMWhat they won’t tell you is that the pharma giants are using your mental health data to push a new agenda. The “brain fog” after cure? Just a side‑effect of secret mind‑control trials. Wake up, people, the truth is hidden in plain sight.
Eric Appiah Tano
October 16, 2025 AT 21:13 PMHey everyone, great discussion! Remember that while the numbers can look scary, many patients see real improvements after treatment. If you’re feeling down, reach out to a support group – shared stories can be a powerful boost.
Jonathan Lindsey
October 17, 2025 AT 16:06 PMOne cannot help but marvel at the irony that, in an era of unprecedented therapeutic breakthroughs, we continue to grapple with the intangible shadows of the mind; indeed, the very notion that a virus, once thought confined to hepatic tissue, can orchestrate a symphony of neuropsychiatric disturbances, is a testament to the intricate interplay of physiology and psychology. It is, therefore, both prudent and profoundly necessary that clinicians adopt a holistic approach-one that seamlessly weaves virological eradication with vigilant mental‑health surveillance-lest we risk reducing a triumph of modern medicine to a mere statistical footnote.
Gary Giang
October 18, 2025 AT 11:00 AMFrom a cultural perspective, the stigma around liver disease can compound the psychological burden; community outreach and education are key to breaking that cycle.
steve wowiling
October 19, 2025 AT 05:53 AMLife is a series of choices, and sometimes the choices we make about our health become philosophical dilemmas-do we treat the virus first or the mind? Either way, ignoring either side is like reading only half of a novel.
Warren Workman
October 20, 2025 AT 00:46 AMLet’s cut the fluff: the cytokine–brain axis is a textbook example of mechanistic pathology. If you’re not measuring IL‑6, you’re missing the primary driver of the mood disturbances associated with genotype 3.
Kate Babasa
October 20, 2025 AT 19:40 PMWhile the data points to heightened inflammatory markers, it is also important to recognize the resilience many patients demonstrate; nuanced support can help translate these findings into tangible improvements.
Shelby Rock
October 21, 2025 AT 14:33 PMi think we should be askin ourselves why we let a virus mess with our thoughts in the first place; maybe it’s a reminder that body and mind ain’t separate rooms, they share the same roof.