Midodrine Dose Timing Calculator
How Timing Affects Your Sleep
Midodrine's half-life is 3-4 hours. Taking your last dose too late can cause alertness, insomnia, and night-time blood pressure spikes. This tool helps you calculate the optimal last dose time based on your desired bedtime.
Your Optimal Last Dose Time
Quick Takeaways
- Midodrine raises blood pressure by stimulating alpha‑1 adrenergic receptors, which can also heighten alertness at night.
- Common sleep‑related side effects include difficulty falling asleep, fragmented sleep, and occasional vivid dreams.
- Timing the dose (usually early afternoon) and pairing it with good sleep hygiene often mitigates insomnia.
- If sleep problems persist, doctors may adjust the dose or switch to alternatives like Fludrocortisone or Droxidopa.
- Monitoring blood pressure and sleep patterns together helps balance symptom relief with restorative rest.
What is Midmidrine and How Does It Work?
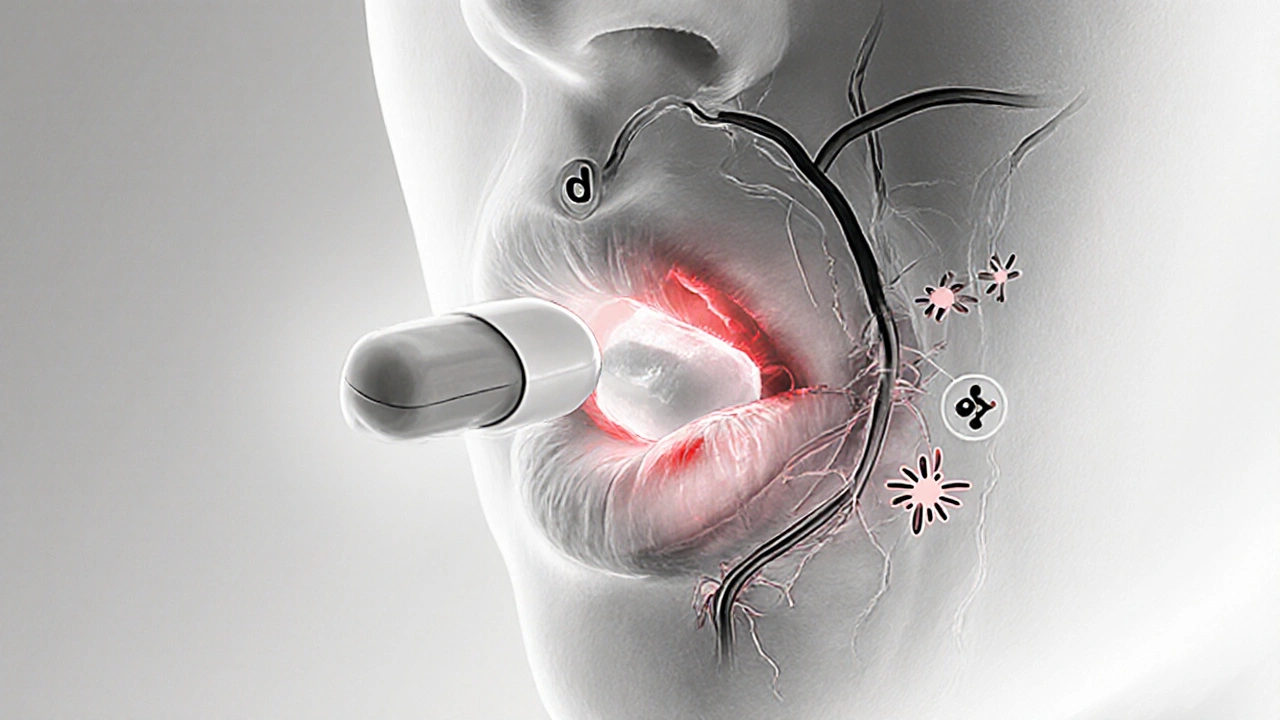
When you first hear about Midodrine is a prescription medication that acts as an alpha‑1 adrenergic agonist to raise blood pressure in people with orthostatic hypotension. It’s taken by mouth, usually in 2‑ to 3‑times‑daily doses. After you swallow a tablet, your liver converts it into the active form, desglymidodrine, which binds to alpha‑1 receptors on blood‑vessel walls.
Those receptors tell the smooth muscle to tighten, narrowing the vessels and pushing blood upward. The result is a steadier blood pressure when you stand, which reduces dizziness, fainting, and the so‑called "standing‑low" feeling.
Because the drug works by stimulating the sympathetic nervous system, it can also increase heart rate and produce a modest boost in overall alertness. That is where the sleep conversation begins.
The Body’s Sleep System: A Brief Overview
Sleep isn’t just “off time” for the brain; it’s a complex series of cycles driven by the circadian rhythm. Your internal clock, set by light exposure, hormones like melatonin, and even body temperature, tells your body when to wind down and when to wake up.
During a typical night you cycle through non‑rapid‑eye‑movement (NREM) stages and then into rapid‑eye‑movement (REM sleep). NREM is restorative, while REM is the stage for vivid dreaming and memory consolidation.
Any drug that nudges the sympathetic nervous system-like Midodrine-can tip this delicate balance, especially if taken too late in the day.
How Midodrine Can Influence Your Nighttime Rest
Most clinical trials focus on the drug’s ability to prevent drops in blood pressure, but a handful of patient‑reported outcomes highlight sleep disturbances. Here’s what tends to happen:
- Increased vigilance: By mimicking the fight‑or‑flight response, Midodrine can make you feel more “on edge,” which translates to a longer time to fall asleep.
- Fragmented sleep: The vasoconstrictive effect may cause occasional spikes in blood pressure during the night, prompting brief awakenings.
- Vivid or unsettling dreams: Some users report unusually intense REM‑phase dreaming, likely tied to the sympathetic surge.
- Night‑time hypertension: For a small subset, the drug’s pressor action pushes blood pressure into the hypertensive range while lying down, which can trigger discomfort and awakenings.
It’s worth noting that not everyone experiences these side effects. Age, dose timing, and personal sensitivity to adrenergic stimulation all play a role.

Identifying Sleep‑Related Side Effects
Because sleep problems can masquerade as “just stress,” it helps to keep a simple log. Track the following for at least a week:
- Bedtime and wake‑up time
- Time you take each Midodrine dose
- Subjective sleep quality (scale 1‑10)
- Any nighttime awakenings, heart‑rate spikes, or headaches
If you notice a pattern-especially a dip in sleep quality after a later dose-you’re probably looking at a drug‑related issue rather than unrelated insomnia.
Practical Strategies to Protect Your Sleep
Fortunately, most clinicians agree that simple timing tweaks can make a huge difference.
1. Schedule the last dose early
Midodrine’s half‑life is roughly 3‑4hours. Taking the final dose before 2pm gives the drug enough time to wear off before you hit the pillow. If you need a third dose for severe symptoms, aim for no later than 4pm and keep the amount low.
2. Pair with a light snack
A modest carbohydrate snack (e.g., a banana or whole‑grain toast) can smooth the blood‑pressure rise and prevent a sudden alertness spike.
3. Optimize sleep environment
Dark, cool rooms (around 65°F) and limiting screen exposure 30minutes before bed support the circadian rhythm. Using a white‑noise machine can also mask any nighttime heart‑rate‑related sounds that might wake you.
4. Consider melatonin
Low‑dose melatonin (0.5mg) taken 30minutes before bedtime can help reset the sleep‑wake cycle, especially if your drug‑induced alertness is mild.
5. Review other meds
Many patients with orthostatic hypotension also take antihypertensive drugs, antidepressants, or beta‑blockers like metoprolol. Those agents can either blunt or exaggerate Midodrine’s effect on sleep. A medication review with your physician can uncover hidden culprits.
When to Talk to Your Doctor
If you’ve tried timing and hygiene tricks for two weeks and still score below a 5 on the sleep‑quality scale, it’s time to bring it up. Your doctor may:
- Lower the dose (e.g., from 10mg to 5mg)
- Switch to an alternative like Fludrocortisone, which works by expanding blood volume rather than direct vasoconstriction.
- Add a short‑acting antihistamine (e.g., diphenhydramine) at bedtime, but only under supervision because of potential next‑day drowsiness.
- Consider a non‑pharmacologic approach such as compression stockings and vigorous hydration, which can reduce the need for higher Midodrine doses.

Comparison with Other Orthostatic Hypotension Treatments
| Medication | Mechanism | Typical Dose | Impact on Sleep | Key Contra‑indications |
|---|---|---|---|---|
| Midodrine | Alpha‑1 adrenergic agonist | 5‑10mg 2‑3×/day | Possible insomnia, vivid dreams, night‑time hypertension | Severe CAD, pheochromocytoma |
| Fludrocortisone | Mineralocorticoid - expands plasma volume | 0.1‑0.2mg daily | Generally neutral; may cause nocturnal edema | Uncontrolled hypertension, heart failure |
| Droxidopa | Dopamine‑β‑hydroxylase substrate → norepinephrine | 100‑600mg 3×/day | Can cause insomnia but less vasoconstriction‑related spikes | Severe cardiac disease, MAO‑inhibitor use |
Choosing the right drug often comes down to a trade‑off between blood‑pressure control and how much it messes with your night. Midodrine tops the list for rapid, predictable pressure elevation, but the sleep‑related side effects are the most prominent.
Bottom Line: Balancing Blood Pressure and Bedtime
Midodrine can be a game‑changer for people who can’t stay upright, yet its sympathetic “boost” can make the brain stay alert when you’d rather be asleep. By timing the dose, watching for nighttime blood‑pressure spikes, and pairing the medication with solid sleep hygiene, most patients can enjoy both stable circulation and a decent night’s rest. If problems linger, a medication review-potentially swapping to Fludrocortisone or Droxidopa-offers a path forward.
Frequently Asked Questions
Can Midodrine cause insomnia?
Yes. Because Midodrine activates alpha‑1 receptors, it can increase alertness and make it harder to fall asleep, especially if taken later in the day.
What is the best time to take my last Midodrine dose?
Most clinicians recommend the final dose before 2pm. If you need a third dose, aim for no later than 4pm and keep the amount low.
Are vivid dreams a sign of a problem?
Vivid or disturbing REM‑phase dreams can be a side effect of the sympathetic surge caused by Midodrine. If they’re frequent or distressing, discuss dose timing or a medication switch with your doctor.
Should I stop Midodrine if I develop hypertension at night?
Don’t stop abruptly. Instead, log your nighttime blood‑pressure readings and bring them to your physician. A dose adjustment or alternative therapy is often enough.
How does Fludrocortisone differ from Midodrine regarding sleep?
Fludrocortisone expands blood volume rather than directly constricting vessels, so it usually has a neutral effect on sleep. However, it can cause fluid retention that may be uncomfortable at night.





Comments
Kevin Adams
October 16, 2025 AT 19:34 PMMidodrine, that little pill that promises to keep you upright, feels like a modern Prometheus stealing fire from the gods of fatigue. Yet, as you swallow it, the alpha‑1 receptors flare like a spotlight on your nervous system, and suddenly bedtime becomes a battlefield, as if a drill sergeant whispered “stand to” into your dreams. It’s a paradox: you chase steadiness in the daylight and sacrifice the sweet surrender of sleep. So, timing isn’t just a recommendation; it’s the truce you negotiate with your own physiology.
Patricia Echegaray
October 17, 2025 AT 17:47 PMWhat they don’t tell you is that pharma companies have a vested interest in keeping you wired, not rested. The same labs that push Midodrine also flood the market with stimulants that keep you buying more prescriptions. Every night you’re a pawn in a larger experiment, a data point for profit motives that thrive on your insomnia. The timing hacks are just a band‑aid, a way to keep the ship afloat while the real agenda sails on.
CHIRAG AGARWAL
October 18, 2025 AT 16:01 PMMidodrine makes me feel like a jittery squirrel at night.
Tom Green
October 19, 2025 AT 14:14 PMYou’re not alone, Chirag. Many patients report that adjusting the last dose to early afternoon and pairing it with a calming routine can dramatically improve sleep quality. Keeping a simple log of dose times and bedtime helps you spot patterns without overcomplicating things. Small tweaks often yield big results, so give it a fair trial before deciding it’s a deal‑breaker.
genevieve gaudet
October 20, 2025 AT 12:27 PMi think the key is to treat midodrine like a coffee – it’s great for a morning boost but you gotta ditch it well before you hit the sack. start tracking the exact minute you take each pill and see how your energy shifts, especially after dinner. a light snack can smooth out the blood pressure spikes and keep you from bouncing off the walls when you try to sleep. also, dim the lights, put away the phone, and let your body know it’s wind‑down time. over time you’ll spot the sweet spot where the drug does its job without stealing your dreams.
Nickolas Mark Ewald
October 21, 2025 AT 10:41 AMLogging your doses and bedtime is a practical step that can reveal the connection between Midodrine timing and sleep quality.
Joanna Mensch
October 22, 2025 AT 08:54 AMThere’s a subtle push from the healthcare system to normalize this wake‑up call at night, framing it as a harmless side‑effect. But we have to ask who benefits when patients stay alert under the guise of “treatment.” The disruption of natural circadian rhythms may have long‑term consequences that aren’t being studied because the focus stays on blood pressure numbers.
Chris Beck
October 23, 2025 AT 07:07 AMData shows that patients who take the final dose after 3pm have a 40% higher incidence of nighttime hypertension. That’s a statistic you can’t ignore, regardless of the marketing fluff.
Emily Rankin
October 24, 2025 AT 05:21 AMWhen you examine the interplay between Midodrine’s pharmacodynamics and the architecture of sleep, a fascinating narrative emerges, one that transcends simple cause‑and‑effect. The drug’s activation of alpha‑1 receptors initiates a cascade that not only constricts peripheral vessels but also stimulates the central nervous system, nudging the brain toward heightened vigilance. In the early evening, this heightened state can delay the onset of NREM sleep, stretching the latency period well beyond the typical 15‑minute window. As the night progresses, sporadic vasoconstrictive surges may trigger brief arousals, fragmenting the restorative deep‑sleep stages that are essential for cellular repair. Moreover, the sympathetic surge can amplify REM intensity, leading to vivid, sometimes unsettling dreams that linger upon awakening. For many patients, these REM perturbations translate into a perceived sense of fatigue even after a full night in bed. The cumulative effect of delayed sleep onset, fragmentation, and intensified dreaming can erode sleep efficiency, reducing the proportion of time spent in the most restorative phases. Yet, the clinical picture is not uniform; younger patients with robust autonomic flexibility often adapt more readily than older individuals whose baroreflex sensitivity wanes. Timing the final dose before the early afternoon, as suggested by numerous protocols, allows the drug’s half‑life to wane, granting the body a smoother transition into the evening’s circadian dip. Complementary strategies, such as low‑dose melatonin, can further coax the pineal gland into resuming its nocturnal melatonin surge, counterbalancing the residual sympathetic tone. Hydration and a modest carbohydrate snack may blunt abrupt blood pressure spikes, smoothing the physiological landscape for sleep. It is also prudent to monitor nocturnal blood pressure trends using a home cuff or ambulatory monitor, thereby detecting any hidden hypertension that could exacerbate sleep disruption. Dialogue with your clinician about dose adjustments or alternative agents, such as Fludrocortisone, should be framed around these objective data points. Ultimately, the goal is a harmonious balance where orthostatic stability does not come at the expense of the nightly restoration that underpins overall health.
Rebecca Mitchell
October 25, 2025 AT 03:34 AMThe sleep‑wake cycle is delicate; even a small shift can ripple through your entire day. Midodrine’s timing matters more than you might think.
Roberta Makaravage
October 26, 2025 AT 01:47 AMExactly! 📊 Keeping a simple spreadsheet of dose times, bedtime, and sleep quality scores is the most efficient way to spot patterns. Trust the data, not the hype! 😎
RJ Samuel
October 26, 2025 AT 23:01 PMOh please, the whole “adjust dose timing” mantra is just a polite way of saying “we haven’t figured out a better drug yet.” If you really wanted seamless sleep, you’d skip the whole alpha‑1 agonist circus and explore non‑pharmacologic lifts like compression stockings or even yoga. The pharma narrative loves to paint timing as a miracle, but it’s really a stopgap.
Sara Werb
October 27, 2025 AT 21:14 PMIt’s infuriating how the establishment sells us a pill that mimics a fight‑or‑flight response, then whispers sweetly about “taking it earlier”. They’re engineering a generation of restless sleepers while cloaking it in clinical jargon, all to keep the profit streams flowing unchecked.
Winston Bar
October 28, 2025 AT 19:27 PMMidodrine, that shiny little tablet, is marketed as a savior for those who can’t stay upright, yet it behaves like a mischievous imp that refuses to let you close your eyes. You pop the dose in the afternoon, hoping the clock will symphonize with your circadian rhythm, but the drug’s lingering alpha‑1 whisper keeps your nervous system on edge well into the night. The result is a cascade of insomnia that gnaws at the edges of your sanity, pulling you deeper into a vortex of fatigue and frustration. Each restless night becomes a reminder that the supposed remedy is also a tormentor, a double‑edged sword that slices through the very rest it promises to protect. When you finally drift off, the sleep is fractured, punctuated by sudden spikes in blood pressure that jolt you awake like an alarm you never set. The vivid dreams that accompany these awakenings are not mere curiosities; they are the brain’s protest against an artificial surge of norepinephrine, manifesting as surreal, often terrifying narratives. Over weeks, this pattern erodes your mood, your concentration, and your willingness to trust any medical solution. The irony is palpable: a drug designed to stabilize your posture ends up destabilizing your mental equilibrium. You begin to suspect that the dosage schedule is a façade, a thin veil draped over the reality that the pharmaceutical industry has not yet engineered a truly sleep‑friendly orthostatic agent. The recommended “last dose before 2 p.m.” feels like a half‑truth, a compromise that still leaves a lingering afterglow of sympathetic activation. Some patients resort to adding melatonin or antihistamines, but these are mere band‑aids on a bleeding wound, masking symptoms without addressing the root cause. In my view, the wiser path is to explore alternatives: fludrocortisone expands plasma volume without the same sympathetic fireworks, and droxidopa offers a different mechanism that may sit more peacefully with sleep architecture. Yet even these alternatives are not without their own specters, reminding us that the quest for a perfect balance is fraught with trade‑offs. Ultimately, the decision rests on a careful weighing of daytime stability against nighttime serenity, a calculus that each patient must perform in consultation with a clinician who truly listens, not just prescribes.
Russell Abelido
October 29, 2025 AT 17:41 PMI hear you, Winston, and I appreciate the depth of your experience. Balancing the need for orthostatic support with sleep quality can feel like walking a tightrope, but collaborative monitoring and incremental dose tweaks often pave the way to a steadier night’s rest.
Katie Henry
October 30, 2025 AT 15:54 PMPlease ensure you discuss any persistent insomnia with your healthcare provider promptly.