For women with polycystic ovary syndrome (PCOS), carrying extra weight isn’t just about appearance-it’s a major driver of hormonal chaos, insulin resistance, and fertility struggles. Many try diet, exercise, and metformin, but often hit a wall. That’s where GLP-1 receptor agonists are changing the game. These drugs, originally designed for diabetes, are now proving to be one of the most effective tools for weight loss and metabolic recovery in obese women with PCOS.
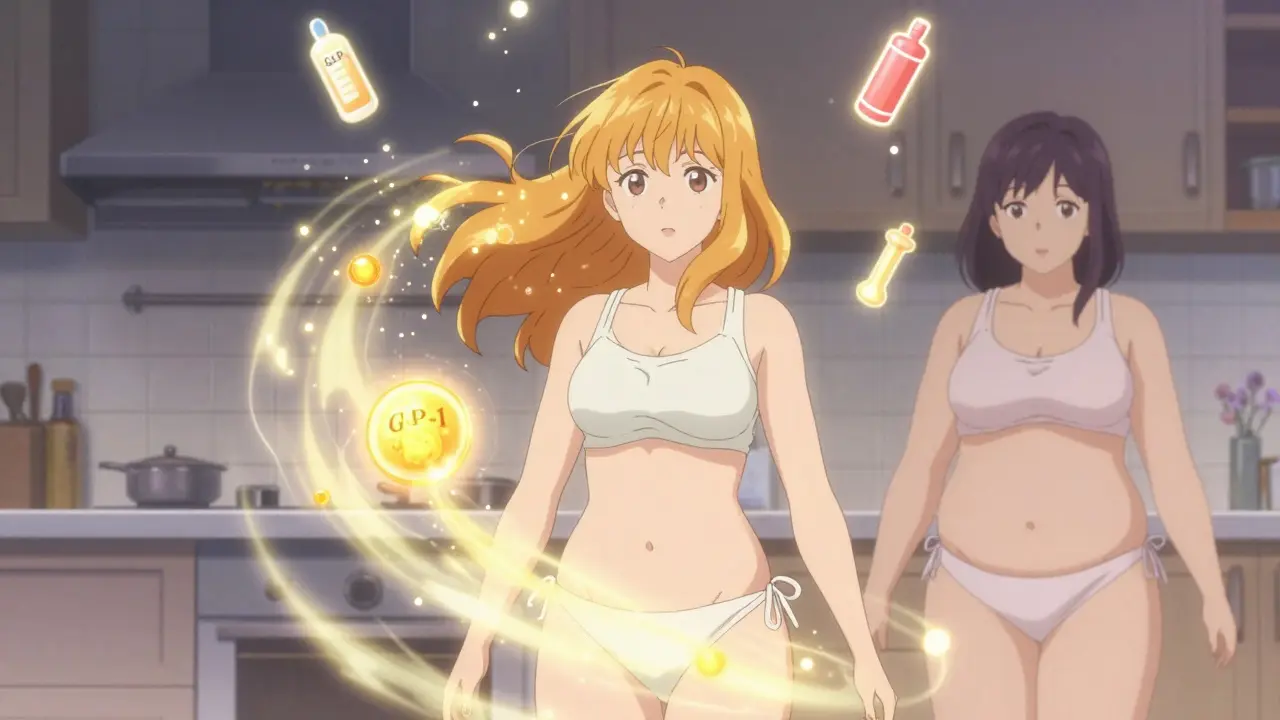
GLP-1s work by mimicking a natural hormone your gut releases after eating. This hormone tells your pancreas to make insulin only when blood sugar is high, slows down digestion so you feel full longer, and sends signals to your brain to reduce hunger. It’s not magic-it’s biology. And for women with PCOS, this biology lines up perfectly with what their bodies need most: less fat, better insulin control, and lower testosterone.
How GLP-1s Actually Work in PCOS
Women with PCOS often have insulin resistance, meaning their bodies don’t respond well to insulin. That forces the pancreas to pump out more insulin, which in turn signals the ovaries to make more testosterone. High testosterone leads to acne, hair growth, irregular periods, and trouble getting pregnant. At the same time, excess fat-especially around the belly-makes insulin resistance worse. It’s a cycle.
GLP-1 receptor agonists break this cycle in three ways:
- Reduce appetite by acting on brain centers that control hunger, making it easier to eat less without constant willpower.
- Slow stomach emptying, so food stays in your gut longer. This helps stabilize blood sugar and reduces cravings.
- Improve insulin sensitivity directly in fat and muscle tissue, lowering the amount of insulin your body needs to produce.
Studies show that after 12 weeks of treatment with liraglutide, obese women with PCOS lost an average of 5-8% of their body weight. With semaglutide, that number climbs to 6-10% in just 6 months. That’s not just a few pounds-it’s enough to reset hormones. Research confirms that losing just 5% of body weight can restore regular periods, lower testosterone levels, and improve ovulation.
Weight Loss Numbers That Matter
Let’s get specific. In one 2024 study tracking 450 women with PCOS and obesity, those taking semaglutide 2.4 mg weekly lost an average of 10.2% of their body weight at 36 weeks. The placebo group? Only 2.1%. That’s a difference of over 20 pounds for someone who weighs 200.
Another meta-analysis of 12 trials found that GLP-1 RAs led to an average weight loss of 3.57 kg (about 7.9 lbs) more than control groups-no diet changes required. That’s not a small boost. It’s clinically meaningful.
But it’s not just about the scale. Visceral fat-the dangerous fat around your organs-dropped by 18% in PCOS patients on semaglutide. Belly fat is especially linked to insulin resistance. Reducing it improves liver function, lowers triglycerides, and reduces inflammation. Blood pressure and cholesterol levels also improved in most studies.
And here’s the kicker: in one study, women who lost weight on GLP-1s saw their testosterone levels drop from 68 ng/dL to 42 ng/dL. That’s the difference between constant acne and clear skin. Between irregular periods and a regular cycle. Between infertility and ovulation.
GLP-1s vs. Metformin: The Real Comparison
Metformin has been the go-to drug for PCOS for decades. It helps with insulin resistance and can lead to 2-5% weight loss. But compared to GLP-1s, it’s like using a spoon to dig a tunnel.
Here’s how they stack up:
| Feature | GLP-1 RAs (Liraglutide/Semaglutide) | Metformin |
|---|---|---|
| Average weight loss (12-24 weeks) | 5-10% | 2-5% |
| Reduction in visceral fat | 15-18% | 5-8% |
| Improvement in insulin sensitivity | Significant | Moderate |
| Effect on testosterone | 20-35% reduction | 10-15% reduction |
| Effect on menstrual regularity | 60-70% of users | 30-40% of users |
| Monthly cost (branded) | $800-$1,400 | $10-$20 |
GLP-1s win on every clinical metric. But cost is a huge barrier. Metformin is generic, safe, and cheap. GLP-1s? Not so much. Many patients can’t afford them without insurance. And even with insurance, prior authorizations can take weeks.

Side Effects: What No One Tells You
Yes, these drugs work. But they’re not gentle. The most common side effects? Nausea, vomiting, constipation, and dizziness. In clinical trials, about 44% of users had nausea, and 24% threw up. For many, it’s mild and fades after a few weeks. For others, it’s unbearable.
One Reddit user wrote: “Spent $1,200 monthly on Wegovy for 4 months. Lost 15 lbs. Couldn’t keep food down. Switched back to metformin.”
That’s not rare. Studies show 15-20% of people stop taking GLP-1s because of side effects. The key is starting low and going slow. Semaglutide usually begins at 0.25 mg weekly and increases every 4 weeks. Liraglutide starts at 0.6 mg daily and goes up over weeks. Rushing the dose increases nausea dramatically.
There are also serious risks. These drugs are not safe if you or a family member has had medullary thyroid cancer. They’re also not approved for use during pregnancy. And while they’re not known to cause pancreatitis, doctors monitor for it.
Who Benefits Most-and Who Doesn’t
GLP-1s aren’t for everyone with PCOS. They work best for women who:
- Have a BMI over 30
- Have insulin resistance or prediabetes
- Struggle with weight despite lifestyle changes
- Want to improve fertility or menstrual cycles
But if you’re a woman with PCOS who’s lean-say, BMI under 25-these drugs likely won’t help much. Studies show little to no benefit in lean PCOS patients. Their hormonal issues aren’t driven by fat, so reducing weight doesn’t fix the root cause.
Also, if you’re not ready to stick with a long-term treatment, GLP-1s aren’t for you. They don’t cure PCOS. They manage it. Stop the drug, and weight often comes back. One 2024 study found that women who stopped both GLP-1s and metformin regained 60-70% of their lost weight in two years. But those who kept metformin after stopping the GLP-1? They only regained one-third.
The Future: What’s Coming Next
The European Medicines Agency accepted Novo Nordisk’s application in June 2024 to approve semaglutide 2.4 mg specifically for PCOS. A decision is expected in early 2025. If approved, this will be the first official indication for GLP-1s in PCOS.
Oral versions of GLP-1s are also in the pipeline. Rybelsus (semaglutide tablet) already exists for diabetes. If proven effective for PCOS, it could replace injections-making adherence easier and stigma lower.
Even more exciting? New drugs like retatrutide, which targets three hormones at once (GLP-1, GIP, and glucagon), are showing 20-25% weight loss in early trials. They may be next-generation tools for PCOS.
By 2027, experts predict GLP-1s will become standard care for obese women with PCOS-especially those with metabolic complications. But access will remain uneven. Without insurance coverage, most patients can’t afford them. And until guidelines fully endorse them, many doctors still hesitate to prescribe.
What to Do If You’re Considering GLP-1s
If you have PCOS and obesity, here’s how to approach GLP-1s:
- Get tested for insulin resistance and prediabetes. A fasting insulin test or HbA1c can help.
- Try lifestyle changes first-diet, movement, sleep. Even small improvements help.
- If you’ve tried everything and still can’t lose weight, talk to an endocrinologist or PCOS specialist.
- Ask about starting low-dose semaglutide or liraglutide. Don’t skip the titration phase.
- Combine it with metformin. Studies show better results and less weight regain.
- Track your symptoms: periods, acne, hair growth, energy levels. Weight isn’t the only win.
And remember: these drugs aren’t a shortcut. They’re a tool. They work best when paired with real, sustainable habits. You still need to eat well, move regularly, and manage stress. The drug just makes it easier.
Can GLP-1s help me get pregnant if I have PCOS?
Yes, for many women. Weight loss from GLP-1s improves ovulation and menstrual regularity. In one study, 42% of women on liraglutide had spontaneous ovulation after 24 weeks. Lower testosterone and better insulin sensitivity create a better environment for fertility. However, GLP-1s are not approved during pregnancy, so you’ll need to stop them if you’re trying to conceive. Always consult your doctor about timing.
How long does it take to see results from GLP-1s for PCOS?
You’ll likely notice reduced appetite and less nausea within the first week. Weight loss typically starts after 4-6 weeks. Most women see meaningful changes in body weight, energy, and skin by 12 weeks. Hormonal improvements-like more regular periods or less facial hair-often appear between 3-6 months. Don’t expect overnight results. This is a slow, steady process.
Are GLP-1s safe for long-term use in PCOS?
Current data shows GLP-1s are safe for up to 2 years. Long-term studies beyond that are still ongoing. The biggest concern is not safety-it’s dependency. Weight often returns after stopping. That’s why experts recommend combining GLP-1s with lifestyle changes and metformin to maintain results. There’s no evidence of organ damage or increased cancer risk in PCOS patients, but monitoring is still advised.
Can I take GLP-1s if I’m not overweight but have PCOS?
Probably not. Most clinical trials and guidelines focus on women with BMI over 30. Lean PCOS patients don’t benefit much because their hormonal issues aren’t driven by fat. GLP-1s work best when insulin resistance is tied to excess weight. If you’re lean, focus on diet quality, exercise, and metformin instead.
Is it worth the cost?
For some, yes. If you’ve tried everything else and your health is suffering-high blood sugar, irregular periods, infertility, or depression-then the cost may be justified. But if you’re unsure, start with metformin and lifestyle changes. If those don’t work after 6-12 months, then consider GLP-1s. Insurance coverage varies widely. Some plans cover them for PCOS off-label; others don’t. Talk to your doctor about patient assistance programs.