Hydration Calculator for Elderly on Diuretics
Hydration Assessment Tool
This tool helps determine your optimal daily water intake based on your age and diuretic type. The ideal range is 1.5 to 2.0 liters daily for most seniors on diuretics.
liters recommended
When you’re over 65 and taking a diuretic for high blood pressure or heart failure, your body is playing a high-stakes game with water. These medications help your heart and kidneys by flushing out extra fluid-but they also make it easier for you to become dangerously dehydrated. And when that happens, your kidneys can shut down in just hours. This isn’t rare. About 20% of hospitalizations in older adults involve dehydration, and those on diuretics are over three times more likely to suffer acute kidney injury than those who aren’t. The scary part? Many seniors don’t even realize they’re dehydrated until it’s too late.
Why Older Adults Are at Higher Risk
Your kidneys change as you age. By the time you’re 70, your ability to concentrate urine drops by half. That means your body can’t hold onto water the way it used to. At the same time, your brain’s thirst signal weakens. Studies show people over 65 feel 40% less thirsty than younger adults-even when their bodies are running on empty. Add to that the fact that 75% of seniors take at least two medications that affect fluid balance, and you’ve got a perfect storm.Diuretics like furosemide and hydrochlorothiazide work by making your kidneys dump sodium and water. But in older kidneys, this process becomes less predictable. A 20mg dose of furosemide that’s safe for a 40-year-old might be too much for an 80-year-old with even mild kidney decline. The American Geriatrics Society recommends cutting standard doses by 30-50% for seniors, yet many doctors still prescribe adult doses out of habit.
The Silent Signs of Dehydration
Dry mouth? That’s not always a reliable clue. In fact, a 2022 survey found that 68% of elderly diuretic users couldn’t name early dehydration symptoms. Many mistake dizziness, fatigue, or confusion for normal aging. But these are red flags.Here’s what to watch for:
- Urine output under 400 mL per day (that’s less than two standard cups)
- Drop in systolic blood pressure by 20 mmHg or more when standing up
- Sudden confusion, disorientation, or slurred speech
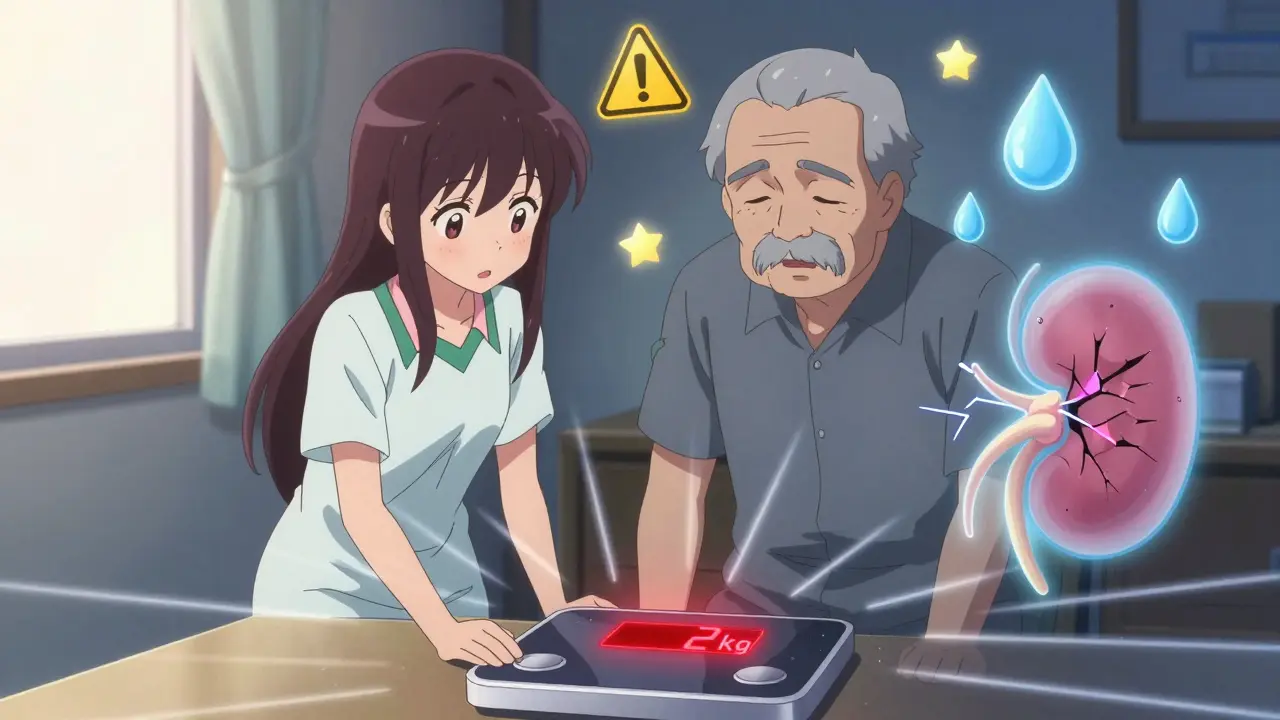
- Weight loss of more than 2 kg (4.4 lbs) in a week
- Dark yellow or amber-colored urine
One caregiver on AgingCare.com shared how her 82-year-old mother’s creatinine jumped from 1.2 to 2.8 in just 48 hours after a day at the beach-even though she’d been drinking water. That’s acute kidney injury. And it’s preventable.
Diuretic Types and Their Risks
Not all diuretics are the same. Each carries different risks:- Loop diuretics (furosemide, bumetanide): Strongest water loss. Used for heart failure. Risk of dehydration is highest.
- Thiazides (hydrochlorothiazide, chlorthalidone): Milder, often for high blood pressure. More likely to cause low sodium (hyponatremia), which can lead to falls and seizures.
- Potassium-sparing (spironolactone, amiloride): Less dehydration risk, but can raise potassium dangerously high-especially in people with kidney disease.
A 2021 JAMA study found hyponatremia occurred in 14% of elderly thiazide users, compared to 8% for loop diuretics. Meanwhile, ACE inhibitors like lisinopril carry 18% lower dehydration risk-but if dehydration does happen, they increase the chance of kidney injury by 22% because they rely on blood pressure to keep the kidneys filtering.
How Much Water Is Enough?
There’s no one-size-fits-all answer. The CKD-REIN study showed a U-shaped curve: too little water (<1 liter/day) and too much (>3 liters/day) both speed up kidney decline. The sweet spot? 1.5 to 2.0 liters daily for most seniors on diuretics.But here’s the catch: spreading that out matters more than total volume. A 2023 study from UCSF found that concentrating 70% of fluid intake between 8 a.m. and 6 p.m. reduced nighttime urination by 41% without raising kidney risk. That’s important because waking up three times a night to pee leads many seniors to cut back on fluids altogether.
Dr. Manjula Karpurapu’s research showed seniors drinking under 1.2 liters daily had nearly five times the risk of hospitalization for kidney injury compared to those hitting 1.5-2.0 liters. Yet, 63% of elderly patients don’t stick to hydration plans. Why? They forget. They’re afraid of incontinence. Or they just don’t know what to do.
Practical Prevention Strategies That Work
You don’t need fancy gadgets. Simple, consistent habits make the biggest difference.- Use marked water bottles. A Home Instead survey found 45% of caregivers reported success using bottles with time-based markers (e.g., “Drink by 10 a.m.”).
- Set phone alarms. A 63% adherence rate was seen when caregivers set hourly reminders for sips of water.
- Eat your water. Watermelon, cucumbers, oranges, and soups count. One study showed 57% of positive outcomes included hydrating foods.
- Check weight daily. A drop of 2 kg or more in a week is a red flag. Call your doctor.
- Test urine color. Pale yellow = good. Dark yellow = drink more. Amber = seek help.
One Reddit user shared that after reducing his dad’s hydrochlorothiazide from 25mg to 12.5mg and adding hourly water sips, his falls dropped from three per month to zero. That’s not luck-it’s management.
What to Avoid
Some well-intentioned actions can backfire.- Don’t “catch up” on fluids after a dry day. Rapid rehydration can cause hyponatremia, especially in diuretic users. A 2023 NHS alert warned that sudden fluid intake can drop sodium levels by more than 10 mmol/L in 24 hours-enough to trigger seizures or coma.
- Avoid NSAIDs. Ibuprofen, naproxen, and other painkillers increase kidney injury risk by 300% in elderly diuretic users. Acetaminophen is safer.
- Don’t assume thirst = need. By the time you feel thirsty, you’re already dehydrated.
- Don’t restrict fluids too much. Fear of incontinence leads many to drink less than 1 liter a day. That’s dangerous.

When to Call the Doctor
If you or a loved one on diuretics has:- Urine output under 400 mL in 24 hours
- Confusion or disorientation
- Sudden dizziness or fainting
- Weight loss over 2 kg in a week
- Swelling in legs or shortness of breath (could mean fluid overload, not dehydration)
Call your doctor or go to urgent care. Acute kidney injury can be reversed-if caught early.
What’s New in 2025
Technology is stepping in. Wearables like the HidrateSpark PRO (FDA-cleared in 2023) track water intake and sync with caregiver apps. The NIH-funded WATER-AGE trial is testing bioimpedance sensors to personalize hydration needs in real time. Early results show a 29% drop in kidney injury episodes.Also, new guidelines expect to recommend cystatin C tests instead of creatinine for seniors. Creatinine can be misleading in older adults because muscle mass declines with age. Cystatin C gives a clearer picture of kidney function.
And while SGLT2 inhibitors like empagliflozin show promise with 24% lower dehydration risk, they cost $550 a month-far more than hydrochlorothiazide at $8. For many, cost still dictates treatment.
Final Takeaway
Diuretics save lives. But they also put kidneys at risk if hydration isn’t managed carefully. The goal isn’t to stop the medication-it’s to support the body while it’s on it. Small, daily actions-like drinking 1.5 liters spread through the day, checking weight weekly, and avoiding NSAIDs-can prevent hospitalization, protect kidney function, and keep seniors independent longer.It’s not about drinking gallons. It’s about drinking smart. And that’s something every caregiver, patient, and doctor can do-today.
Can elderly people on diuretics drink too much water?
Yes, but it’s rare. Drinking more than 3 liters daily can strain the kidneys, especially in those with advanced kidney disease (stages 4-5). The European Renal Association warns that excess fluid can cause pulmonary edema in these patients. The goal is balance: 1.5-2.0 liters daily is optimal for most. Too little increases dehydration risk; too much can worsen heart or kidney conditions. Always follow your doctor’s guidance based on your kidney function.
How often should seniors on diuretics get blood tests?
Every 3 to 6 months for basic electrolytes (sodium, potassium, creatinine). More frequent testing (every 1-2 weeks) is needed when starting a new diuretic, changing doses, or after illness like diarrhea or vomiting. The 2023 NICE guidelines stress that routine monitoring prevents silent kidney damage. Some doctors now use cystatin C, which is more accurate than creatinine in older adults.
Is it safe to skip a diuretic dose if I’m not feeling well?
Never skip a diuretic dose without talking to your doctor. If you’re dizzy, nauseous, or have diarrhea, you may be dehydrated-but stopping the diuretic won’t fix it-and could make heart failure worse. Instead, drink small sips of water, check your weight, and call your provider. They may adjust your dose or suggest temporary fluid support. Self-adjusting medications can lead to dangerous fluid buildup or kidney injury.
What’s the best way to remind an elderly person to drink water?
Use a combination of tools. Marked water bottles with time labels (e.g., “Drink by 10 a.m.”) work well. Set phone alarms every 2 hours during waking hours. Apps like HidrateSpark sync with smart bottles and send alerts to caregivers. Eating water-rich foods like watermelon, soups, and cucumbers also helps. The key is consistency-not relying on thirst. Caregivers report 63% adherence with scheduled reminders.
Can dehydration from diuretics cause permanent kidney damage?
Yes, repeated episodes of dehydration can lead to chronic kidney damage. Each acute kidney injury (AKI) episode increases the long-term risk of progressing to kidney failure. The CKD-REIN study showed that even one episode of AKI in seniors on diuretics raises the risk of future kidney decline by 35%. Prevention is critical: keeping hydration between 1.5-2.0 liters daily and avoiding NSAIDs can protect kidney function for years.
Are there alternatives to diuretics for seniors with high blood pressure?
Yes. ACE inhibitors, calcium channel blockers, and ARBs are often used instead or alongside diuretics. ACE inhibitors carry 18% lower dehydration risk but increase AKI risk during dehydration. SGLT2 inhibitors (like dapagliflozin) are newer options with lower dehydration risk and added heart benefits-but they’re expensive. The best choice depends on kidney function, heart health, and cost. Always discuss alternatives with your doctor before switching.
For caregivers: The most effective intervention isn’t a pill-it’s a routine. Make hydration part of the day, like brushing teeth. For seniors: Don’t wait until you’re thirsty. Sip. Check. Call. Your kidneys will thank you.






Comments
Marilyn Ferrera
December 31, 2025 AT 16:18 PMDehydration isn't just 'not drinking enough'-it's a silent, systemic collapse waiting to happen. And we treat it like a lifestyle choice. We blame the elderly for forgetting water, but we don't install reminders, don't adjust meds, don't monitor weight. It's negligence dressed as 'normal aging.' And it kills.
Stewart Smith
January 2, 2026 AT 07:32 AMSo… we’re saying the solution is to drink water like it’s a job? Cool. I’ll just set 12 alarms and eat watermelon like it’s my pension. Meanwhile, my aunt’s doctor still prescribes 25mg of HCTZ like she’s 50. 😅
Retha Dungga
January 3, 2026 AT 14:50 PMwater = life 🌊 but also… why is everyone so scared of peeing?? like… we’re all just leaking souls and afraid to let go 💔 #hydrationislove
Jenny Salmingo
January 4, 2026 AT 19:21 PMMy mom drinks water when I remind her. I put a bottle by her chair. She drinks it. No alarms. No apps. Just me saying, 'Mom, sip.' It works. Simple.
Aaron Bales
January 6, 2026 AT 14:12 PMStop blaming patients. Doctors are the problem. They don’t adjust doses. They don’t check creatinine properly. They don’t know the difference between loop and thiazide risks. Fix the system, not the senior.
Martin Viau
January 6, 2026 AT 17:11 PMOf course Americans are dehydrated-your water’s overchlorinated, your diet’s processed, and your doctors still think 'drink eight glasses' is medical advice. Meanwhile, Canadians hydrate with maple syrup tea and know better. This is a cultural failure.
Robb Rice
January 7, 2026 AT 10:44 AMWhile the intent of this post is commendable, it is riddled with syntactical inconsistencies-particularly in the use of em dashes and inconsistent capitalization after colons. Additionally, the reference to 'HidrateSpark PRO' as 'FDA-cleared in 2023' lacks citation. A more rigorous editorial review would elevate its credibility.
Harriet Hollingsworth
January 8, 2026 AT 06:47 AMSome people think this is about water. It’s not. It’s about control. We let old people die quietly because we don’t want to clean up after them. We don’t want to change the meds. We don’t want to pay for cystatin C tests. We just want them to stop being a burden. And that’s the real crime.